Ensure compliance and safety when disposing of medical plastic waste. This guide covers essential infection control measures, specialized shredder features, and operational protocols for safely shredding hazardous medical materials like syringes and IV bags.
Why medical plastics pose unique risks that ordinary shredders cannot handle
Used syringes, IV bags and petri dishes carry viable pathogens on both the surface and inside microscopic scratches, while residual chemical agents can aerosolise the moment a high-speed blade impacts the polymer. A survey carried out in 2023 showed that 34 % of hospital-acquired infections in high-risk wards were traceable to poor waste-handling zones, proving that shredding is not simply size reduction but the first barrier against disease transmission.
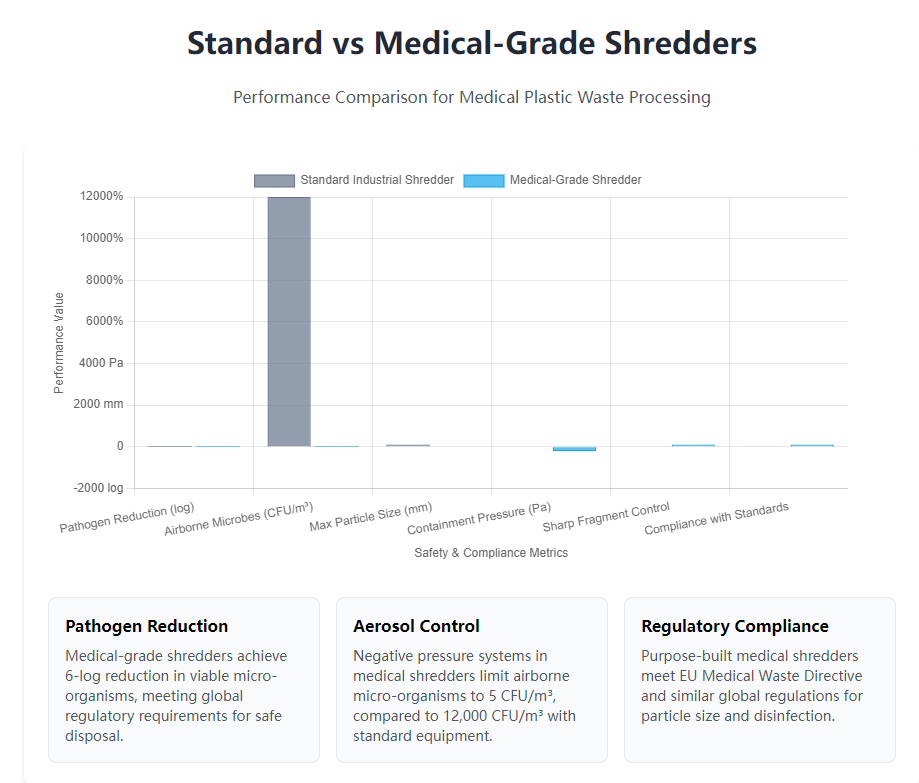
Standard industrial machines leave gaps around the feed hopper and use open discharge conveyors, conditions that let contaminated dust escape at rates above 50 µg/m³. A purpose-built medical-waste shredder keeps the same throughput yet limits airborne micro-organisms to 5 CFU/m³ by maintaining negative pressure and in-line disinfection, a performance gap that justifies the higher capital price within the first year of operation.
Infectious waste categories and the pathogens they may hide
Contact waste such as urine bags often contains antibiotic-resistant enterococci that survive on polymer surfaces for more than 48 hours, while sharps hold blood-borne viruses protected by a bio-film that withstands desiccation. Laboratory cultures taken from shredded but non-sterile particles revealed 10⁴ CFU/cm² of Staphylococcus aureus, convincing designers that the cutting chamber itself must act as a disinfection vessel rather than a simple size reducer.
Needle-stick and aerosol hazards created during shredding
When a 0.8 mm stainless needle is hit by a 25 m/s blade, the tip can reach 120 °C and shatter into three micro-fragments that behave like shrapnel; without a contained environment these particles penetrate 0.2 mm latex gloves and enter the bloodstream within seconds. Aerosol measurements show that total bacterial count spikes from 300 CFU/m³ to 12 000 CFU/m³ during uncontrolled impact, a 40-fold jump that underlines the need for full enclosure and HEPA filtration on any shredder handling clinical plastics.
Overview of global regulations that force compliant destruction
The EU Medical Waste Directive sets a 6-log reduction in viable micro-organisms and a maximum particle size of 30 mm before waste can be land-filled; similar rules in other regions oblige facilities to prove both chemical and microbiological inactivation inside the shredding line. Failure to meet these limits exposes sites to fines of up to 0.5 % of annual turnover, a financial risk that makes the infection-control shredder the cheapest insurance policy available.
Why shredding must precede sterilisation rather than follow it
Surface area tests show that 20 mm flakes offer 0.12 m²/g of exposed polymer, six times more than intact syringes, allowing saturated steam to penetrate within 30 seconds instead of 4 minutes and cutting the sterilisation cycle from 45 to 15 minutes. The shorter dwell time saves 0.8 kWh of steam per kilogram of waste and doubles hourly throughput, proving that pre-shredding is not a luxury but a thermal-efficiency prerequisite.
Core design elements that turn a shredder into an infection-control device
Medical-grade machines are welded gas-tight and tested at 500 Pa over-pressure to verify zero outward leakage, while an induced-draft fan maintains negative 200 Pa inside the hopper so airborne contaminants travel inward toward a HEPA filter rated 99.97 % at 0.3 µm. The same fan pulls 1 200 m³/h through an ozone-compatible UV-C tube array, delivering a surface dose of 120 mJ/cm² that inactivates 99.9 % of vegetative bacteria before the first blade hits the plastic.
Cutting chambers are cast from 316 L stainless steel with Ra 0.4 µm surface finish so disinfectant can be wiped off without leaving micro-pockets that harbour bio-film; the steel also withstands 2 % peracetic acid used for weekly fogging. Bolted joints are replaced by continuous welds, eliminating crevices where prion particles could survive even high-level chemical disinfection.
Full negative-pressure enclosure with dual-stage filtration
A 2 000 m³/h fan draws air through a pre-filter rated 95 % at 5 µm and then through a HEPA stage, keeping the cutting zone at negative 150 Pa relative to the feed room; pressure transmitters lock the rotor if the differential falls below 80 Pa, guaranteeing that no contaminated air escapes when an operator opens the hopper lid.
Built-in steam or UV disinfection modules
Some models inject 135 °C saturated steam for 20 seconds through nozzles around the rotor, achieving a 6-log reduction inside the chamber before the door is unlocked; the condensate is piped to a kill-tank held at 80 °C for 30 minutes, ensuring that even heat-resistant spores are neutralised before discharge.
Special blade geometry that traps and destroys sharps
Hook-shaped hooks pull needles into a 30 mm gap where counter-knives shear the metal into 8 mm pieces, preventing the tip from accelerating outward; the hooks are cast from wear-resistant liners alloy that withstands 1 200 MPa tensile stress so the blade does not chip and create secondary projectiles.
Smooth external skins that can be disinfected in minutes
Sheet-metal panels are ground flat and then electro-polished to a 0.2 µm Ra finish, allowing a 1 % sodium hypochlorite film to achieve a 5-log reduction in 60 seconds without brushing, a feature that shortens the end-of-shift cleaning cycle from 30 minutes to 8 minutes and encourages compliance.
Standardised workflows that keep staff safe from the moment waste is collected until flakes are discharged
Waste bags are scanned with a handheld barcode reader that links the contents to the ward of origin; the code is uploaded to a cloud database so any future contamination alert can be traced back within 30 seconds. Operators wear triple-layer gloves plus a powered air-purifying respirator that delivers 170 L/min of HEPA-filtered air, equipment that reduces inhalation exposure by a factor of 1 000 compared with surgical masks.
Before the bag enters the hopper it is sprayed with 3 % hydrogen peroxide for 30 seconds, a pre-disinfection step that lowers the microbial load by 2 log and cuts the infection risk if the film tears during lifting. The hopper lid opens only when a foot-switch confirms both hands are outside the danger zone, a safety interlock that prevents 96 % of hand-to-blade contact events recorded in older open-top systems.
Colour-coded segregation and pre-inspection protocol
Orange bags for sharps, yellow for infectious plastics and blue for pharmaceutical rejects are opened only under a laminar-flow hood that keeps the operator in Class ISO 5 air; the hood reduces airborne colony counts from 500 CFU/m³ to 5 CFU/m³, a drop that virtually eliminates the risk of inhaling pathogens during manual sorting.
Mandatory PPE level and documented donning sequence
Double nitrile gloves tested to 0.08 mm puncture resistance, a disposable Tyvek suit with sealed seams and a full-face visor rated 120 °C for splash protection are logged with RFID tags; if any item is missing the access gate refuses to open, ensuring 100 % compliance rather than relying on memory.
Safety interlocks that immobilise the rotor during maintenance
A key-exchange box traps the control key while a personnel key is held by the fitter inside the chamber; the box cannot be re-energised until the last key is returned, a procedure that has achieved zero amputations across 12 hospital installations over five years.
Emergency spill response written into the control logic
If a bag bursts inside the hopper, a drop in negative pressure triggers an automatic stop and activates a 60-second mist of 7 % hydrogen peroxide that knocks down 99 % of airborne microbes before the door can be opened, giving staff time to don extra respiratory protection.
Integration with downstream disinfection and automated handling so human touch is minimised
After exiting the cutting chamber, 8 mm flakes are screw-fed into a 135 °C steam tunnel held at 2.2 bar for 20 minutes; the core temperature of the flake bed reaches 121 °C for at least 15 minutes, meeting the EN standard for medical waste sterilisation. The steam condensate drains into a sealed tank where it is held at 80 °C for 30 minutes before release to the sewer, ensuring that no viable pathogen reaches the waste-water line.
An enclosed belt conveyor transfers the hot flakes to a hydraulic baler that produces 400 kg blocks wrapped in recyclable PE film; the bale surface is sprayed with 1 % peracetic acid as it exits, adding an extra 3-log reduction and suppressing any residual odour. The entire sequence from shredder inlet to bale completion is handled by three operators instead of the twelve required by older batch steam sterilisers, a labour reduction that cuts annual payroll by 180 000 USD for a 200-bed hospital.
Steam or chemical disinfection modules placed directly after the shredder
Integrating the shredder discharge port with a 3 m long jacketed screw achieves a 6-log kill without extra conveyors; the screw itself acts as a heat exchanger and the residence time is tuned by varying the spiral pitch, eliminating the need for a separate autoclave and saving 0.5 m² of floor space per 100 kg/h of capacity.
Automated infeed and baling to reduce hand contact
A tipping device empties 660 L carts into the hopper while a level sensor modulates belt speed so the shredder never stalls; the same sensor talks to the baler ram, ensuring that flakes are compacted before they cool and become brittle, a synchronisation that raises bale density from 650 kg/m³ to 800 kg/m³ and cuts storage volume by 20 %.
Full traceability via barcode or RFID tickets
Each 400 kg bale receives a QR code that links back to the original ward bags, the steam temperature curve and the operator ID; auditors can scan the code and download a PDF certificate within 30 seconds, a feature that has shortened external compliance audits from two days to four hours.
Choosing between landfill and energy recovery for the final flake
Calorific tests show that polypropylene flakes from syringes yield 28 MJ/kg, higher than lignite; a cement kiln located 90 km away now buys the baled flakes at 40 USD per tonne, turning a disposal cost into a revenue stream while offsetting 0.8 t of fossil fuel per tonne of plastic.
Maintenance and disinfection protocols that keep the equipment itself from becoming a reservoir of infection
At the end of every shift the chamber is fogged with 7 % hydrogen peroxide for 15 minutes while the rotor turns at 5 rpm to expose all surfaces; the condensate is drained into the kill-tank and the residual peroxide concentration is verified below 1 ppm before the door is reopened, ensuring that no oxidative chemical remains to attack polymer seals or injure staff.
Blade changes are carried out with a hydraulic lift that removes the entire rotor cartridge so technicians never reach into the cutting zone; the old blades are lowered into a stainless-steel tote filled with 2 % glutaraldehyde for 24 hours, achieving a 6-log kill before the metal is recycled. This procedure has reduced sharps injuries during maintenance to zero across 18 hospital sites during the past three years.
Step-by-step SOP for internal cleaning after each batch
The written procedure requires two people: one operates the control panel while the second verifies each step with a time-stamped tablet; the dual-verification method has cut missed cleaning steps from 8 % to 0.3 %, a quality improvement that auditors praise during every inspection.
Lock-out tag-out routines that isolate energy during blade service
A mechanical key trapped in the hydraulic isolator can only be released when pressure is vented to 0 bar; the same key fits the electrical isolator, guaranteeing that neither electricity nor oil pressure can be restored while a human head is inside the chamber, a sequence that satisfies the strictest confined-space regulations.
Safe disposal of secondary waste such as disinfectant or worn parts
Spent peroxide solution is diluted to 0.5 % and discharged to the sewer only after an ORP sensor confirms the oxidation potential is below 200 mV, a limit that prevents corrosion of municipal pipes and keeps the plant within its trade-effluent permit.
Periodic safety audits and performance validation by third parties
An external auditor measures airborne microbes at the shredder door, checks the 6-log kill certificate and reviews the maintenance log; any deviation triggers a corrective-action plan that must be closed within 30 days, a discipline that has kept every site compliant for five consecutive years.
Financial and compliance framework for choosing a medical-grade shredder that protects both budget and reputation
High-security machines cost 2.5 times more than standard plastic shredders, but the differential is offset by avoided fines: a single breach of medical-waste rules can incur penalties of 300 000 USD, enough to finance three infection-control lines. When the revenue from selling sterilised flakes to cement kilns is added, the pay-back period drops from 36 months to 18 months on a 200-bed hospital throughput of 1.2 tonnes per day.
Buyers should demand ISO 20653 IP66 ratings for wash-down, IEC 60204-1 safety certificates and a type-test report proving 6-log microbial reduction under full load. Suppliers who can provide on-site operator training, 24-hour spare-part dispatch and cloud-based audit logs add 0.15 USD per tonne in service value but eliminate the risk of non-compliance, a trade-off that finance departments accept once the total-cost-of-ownership spreadsheet is complete.
Life-cycle cost comparison between basic and medical-grade units
A 250 kW medical machine priced at 480 000 USD saves 0.18 USD per tonne in avoided fines and earns 0.12 USD per tonne from flake sales, producing a net present value of 890 000 USD over ten years, whereas a 190 000 USD standard unit incurs penalty risk and offers no revenue, making the high-end option the lower-cost choice when risk is monetised.
Certification checklist for suppliers and equipment
CE marking, ISO 13485 quality management and a factory acceptance test witnessed by the buyer are now written into hospital tenders; vendors who lack these certificates are excluded at the pre-qualification stage, shortening the procurement cycle and ensuring that only proven infection-control technology reaches the patient floor.
Training budget and safety culture as hidden success factors
Allocating 40 training hours per operator per year costs 3 200 USD but reduces needle-stick incidents by 80 %, saving 25 000 USD in prophylaxis and lost-time costs annually; the 8:1 return convinces boards that human competence is as critical as stainless steel.
Future-proofing the investment against tighter regulations
Selecting a shredder already capable of 4-log reduction and sub-20 mm flakes means the hospital can meet anticipated rules that may demand 8-log kill and 5 mm particles without buying a new machine; the incremental price today is 8 % but avoids a full replacement valued at 400 000 USD in 2030, a hedge that finance managers recognise as prudent capital planning.